DNAP student travels to Haiti with medical relief team
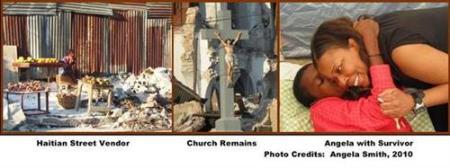
The following is a piece written by former Texas Wesleyan student Angela L. Smith, CRNA, DNAP, about her travels to Haiti in 2010 to provide medical aid.
After hearing the alarming stories regarding the lack of anesthesia supplies and personnel in Haiti, our chief anesthesiologist, Dr. Nagaraj Kikkeri of White Rock Anesthesia Group in Dallas, began the tedious task of making travel arrangements to Haiti. We quickly learned that commercial air was not an option and that volunteer medical relief organizations were only interested in individuals with prior affiliation and experience in emergency medical relief. Eventually, Dr. and Mrs. Kikkeri managed to make contact with Grace Flights, an organization which provides transportation for family members facing medical emergencies.
Our initial journey to Haiti began on January 18, 2010, just six days after the devastating earthquake. Because private travel into Port au Prince was off limits at the time, we decided to land in Jacmel which is located approximately two hours southeast of Port au Prince. The area was in desperate need of medical supplies and personnel but without adequate shelter and equipment in which to provide care.
Our group, along with several surgeons and nurses from Houston, Texas reluctantly boarded U.S. Air Force helicopters and traveled to the Port au Prince airport the next day. From there, we traveled to the CDTI hospital. During the thirty minute trip through downtown Port au Prince, we got our first glimpse of the devastation and soon realized that the magnitude of the situation was far worse than any of us could have imagined.
In the wake of disaster
At this time, the "tent cities" were beginning to multiply rapidly throughout the city but many families seemed reluctant to leave the areas where their homes once stood. As we slowly made our way to the hospital with our supplies on the back of the pick-up truck, I saw helplessness, extreme hunger, thirst and despair, but not one act of violence.
As a result of my military training, I understood the concept of battlefield triage and delivery of care; however, nothing could have prepared me for this experience. Immediately upon arrival to the hospital, we were given a quick tour and immediately went to work. My group was assigned to the emergency room/operating room where three to four surgeries were in progress at all times.
Because the oxygen supply was scarce, general anesthesia was not an option; thus, we were forced to perform nerve blocks supplemented with intravenous sedation, which worked well. In some of the make shift hospitals in the area, the ability to provide any type of anesthesia was lacking and many procedures were performed with little or no anesthesia. One surgeon reported that whiskey was being used as a numbing agent and to fight infection.
On our second day at the hospital, we encountered a 44-year-old woman with a severe scalp laceration. Upon admission to the hospital, she had been brought to surgery and the plan was to clean and suture the site, but when the bandages were removed, maggots were found inside the wound. As a result, she was taken outside and classified as "expectant", a triage term used to classify individuals who are not expected to survive. We learned that the woman had not received medical treatment, food or water for three days; however, she was lucid and able to communicate with us appropriately. Because resources were limited and evacuations were being reserved for children and younger adults, this patient was not a candidate for immediate care. As a result of media attention and persuasion of the Canadian government, she was finally evacuated to Martinique, Canada. Many believe that the maggots were the reason for her survival.
The majority of the procedures performed at CDTI were orthopedic in nature, mostly amputations. For me, the most disheartening reality was the fact that one half of the amputations involved children and that many of the amputations could have been prevented if the appropriate orthopedic equipment was available.
From bad to worse
On January 21, which happened to be my birthday, our worst fears were realized. An aftershock registering 6.0 occurred in the early hours of the morning. In the midst of the chaos, a little boy who had recently undergone a leg amputation was so afraid that he tried to run in spite of the fact that he only had one leg. Later that day, while in the operating room another aftershock shook the building and some of the cracks in the walls became wider right before our eyes. At this point, all surgeries were postponed while the building underwent inspection.
Our second visit to Haiti came about as a result of the impending departure of the French medical team, which had taken responsibility of all medical operations at the hospital after we left.
While a group of American surgeons were due to arrive prior to their departure, replacements for anesthesia services were questionable. Again, we managed to obtain transportation through Grace Flights directly into Port au Prince. Armed with an abundance of anesthetizing agents and other supplies we arrived to find that conditions within the hospital had improved a great deal; however living conditions within the city and surrounding areas had not improved very much.
During this trip, only one amputation was performed and the majority of the surgical procedures involved follow-up care, a few revisions of previous amputations, wound irrigations and skin grafts. Another noticeable improvement was that the "recovery room", which initially consisted of a few tents in the parking lot with post-operative care provided by the family members of the wounded, was now being staffed around the clock by trained nurses and that every patient had some form of shelter.
Lingering concerns
While some improvements were noted during our second trip, several concerning issues come to mind: placement of the orphaned or displaced children and the rainy season which is rapidly approaching. With regard to the orphaned children, adoptions are projected to take two years in order to insure that efforts to locate family members have been exhausted. In the meantime, with the government in chaos, who will protect the children?
Adequate shelter is a very serious issue in Port au Prince. In one of the tent cities, there are an estimated 100,000 individuals. Many of these tents are made from bed sheets and offer very little protection from the rain. In light of the lack of sanitation and the undetermined number of bodies which remain buried beneath the buildings, the rainy season also presents an opportunity for the spread of disease.
Angela L. Smith, CRNA, DNAP
Master of Science in Nurse Anesthesia, Texas Wesleyan Class of 2001
Doctorate of Nurse Anesthesia Practice, Texas Wesleyan Class of 2012
Major, U.S. Army Nurse Corps (Reserves)
"In as much as you have done unto the least of these...."







